Understanding the Bristol Stool Chart: A Guide to Identifying Your Stool Type
Key takeaways:
The Bristol Stool Chart is a system to identify abnormal and normal stools based on appearance and consistency.
It’s used by both healthcare professionals and researchers, allowing for better patient communication and uniform scientific analysis.
Types 3 and 4 on the Bristol Stool Chart indicate healthy digestion and defecation, while the other types point to problems.
The 7 Types of Stool on the Bristol Stool Chart
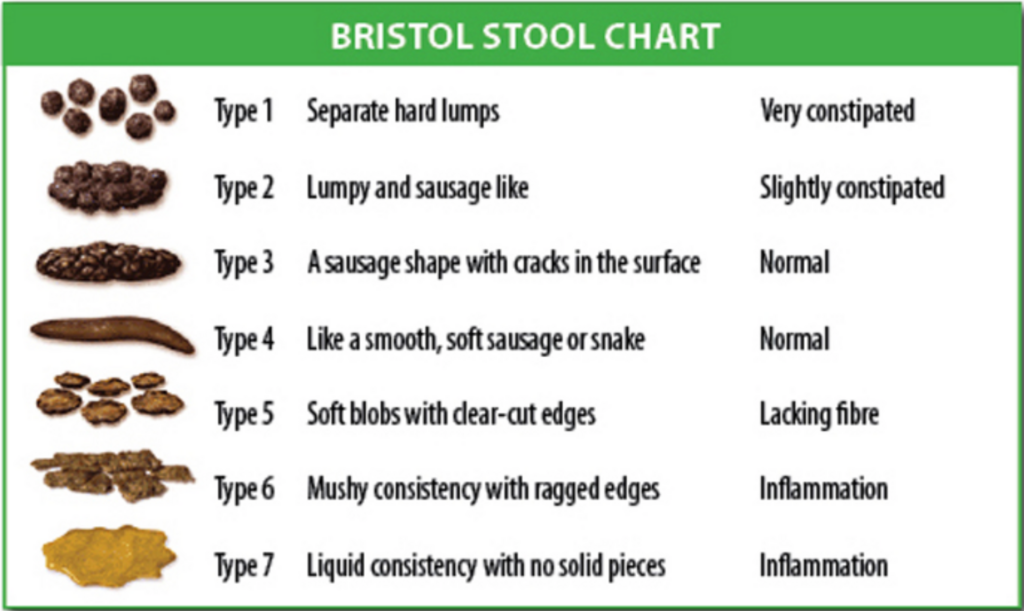
Type 1: Separate Hard Lumps
Type 1 stools are solid pieces of hard, lumpy, poop. They’re challenging to pass, indicating significant constipation and a need to increase your fiber intake. Constipation can cause nausea, discomfort, and bloating.
Incorporating more fruits, vegetables, and whole grains into your diet can help soften your stools, making them easier to pass.
Type 2: Lumpy and Sausage-Shaped
Type 2 stools, though slightly easier to pass than type 1, can still suggest constipation. These lumpy, sausage-shaped stools may require some straining to get out.
Increasing your fiber and water intake can help soften these stools, making them easier to evacuate.
Type 3: Sausage-Shaped with Cracks
Type 3 stools are ideal stools that signify a healthy digestive system. Well-formed and smooth, with cracks on their surface, these stools reflect a balanced diet and good digestive health.
In other words… great job!
Type 4: Smooth and Soft Snake-Like
Type 4 stools resemble type 3 stools but are smoother and softer. These healthy stools are easy to pass and also signal a digestive system functioning normally.
Type 5: Soft Blobs with Clear Edges
Type 5 stools are soft with clear-cut edges and generally easy to pass. They can suggest a diet high in fiber and hydration.
Because type 5 stools are softer than the ideal stool, consult your doctor if you frequently experience this type of stool along with discomfort or other GI symptoms.
Type 6: Mushy with Ragged Edges
Type 6 stools are fluffy pieces with ragged edges. Mushy stool hints at possible inflammation in the digestive tract or a high-fat diet.
If you consistently have type 6 stools, talk to your doctor. They may recommend dietary changes or additional testing to determine what’s causing inflammation. Brief bouts of diarrhea may be treated with over-the-counter medications like Pepto-Bismol.
Type 7: Watery and Liquid
Type 7 stools are entirely liquid, signifying diarrhea or other digestive issues. Diarrhea often happens because of too-fast transit time (the speed at which your digestive system passes waste), dehydration, or a variety of medical issues like infections.
If you consistently have type 7 stools, consult your doctor. Diarrhea can indicate a more severe condition, especially when accompanied by noticeable amounts of mucus, stomach pain, a burning sensation, or blood in your stool.
The History of the Bristol Stool Chart
The Bristol Stool Chart (sometimes referred to as the Bristol Stool Form Scale) was created in 1997. The chart provides a practical tool for patients and medical professionals to categorize various types of poop.
First introduced by Dr. Ken Heaton, a gastroenterologist in Bristol, UK, the chart is now recognized and used globally in research related to gastrointestinal function.
Dr. Ken Heaton and the Development of the Chart
Dr. Ken Heaton, a distinguished gastroenterologist, dedicated years to researching and analyzing stool types and their implications for digestive health. He realized that people often found it challenging to accurately describe their stool, leading to confusion and misdiagnoses.
Recognizing the need for a better system, Dr. Heaton developed the Bristol Stool Chart, breaking down the visual appearance of stool into 7 distinct types.
Dr. Heaton’s work in creating the Bristol Stool Chart transformed the way both medical professionals and patients discuss digestive health. The chart has become a fundamental tool in gastroenterology.
The Chart’s Impact on Medical Research
The Bristol Stool Chart has proven to be a valuable tool in medical research. Many studies use the chart to evaluate gastrointestinal symptoms and treatments. Over time, it’s developed a reputation as a reliable and user-friendly method for describing poop characteristics.
Here are a few examples of notable studies and meta-analyses that rely on the Bristol Stool Chart for identifying feces:
- A 2013 systematic review on how useful probiotics can be for treating diarrhea caused by radiation therapy
- A 2020 meta-analysis of studies about how acupunture impacts IBS symptoms
- A 2022 systematic review on the effect of Traditional Chinese Medicine (TCM) on functional constipation
- A 2022 report on the best way for primary care providers to discuss stool with patients
The Importance of Monitoring Your Stool
By keeping an eye on your stool, you can identify potential digestive problems before they get worse. Noticeable changes in the frequency, consistency, and color of your poop may all indicate that your digestive system is not functioning at its best.
Digestive Health and Stool
The color, consistency, and shape of your poop indicate a lot about your digestive health.
For example, watery or loose stools might suggest diarrhea, an infection, or another digestive issue. In contrast, hard, lumpy stools could signal constipation or a diet deficient in fiber.
Understanding the different types of stool lets you and your healthcare provider identify problems and make necessary adjustments to your diet and lifestyle.
And it’s not just the color and shape — the odor of your stool can also hint at potential health concerns.
A strong, unpleasant smell (or, in some cases, sweet-smelling stool) might suggest an infection or malabsorption problems. An absence of odor may indicate that your digestive system isn’t producing sufficient stomach acid to break down food effectively.
Identifying Potential Health Issues
Understanding your stool type, color, and odor is the first step to diagnosing potential digestive problems and seeking proper medical attention. In some cases, changes to the color of your stool are normal.
Here are a few examples of what poop changes mean:
- Tarry, black stool is sometimes a sign of internal bleeding.
- Unexplained blood in your stool may point to hemorrhoids or inflammatory bowel disease (IBD).
- Pale or clay-colored stool (sometimes referred to as yellow poop) might signify liver disease.
- Iron supplements may cause black or dark green stool.
- Antibiotics can result in loose or watery stools.
When you monitor your bowel movements and stool appearance, you can catch symptoms of problems early while noting how your diet or supplements alter your poop in expected ways. If you notice significant changes, seek medical attention from a qualified provider.
(Yes, it might seem gross to pay close attention to your bowel habits. But we promise — it’s good for you!)
Factors Affecting Stool Consistency and Appearance
Diet and Nutrition
A diet rich in fiber and balanced in carbohydrates, proteins, and fats is crucial for good digestive health. Insufficient fiber intake can lead to constipation, hard stools, and other digestive issues.
What you eat also has a tendency to change the color of your stool. Eating beets might make your stool red, while eating bright green cupcakes might result in green poop.
Specific foods, such as spicy or greasy meals, may also trigger digestive problems for some people.
Hydration
Proper hydration is essential for maintaining healthy digestive function. Insufficient water intake can result in constipation and hard stools, as the digestive process requires a lot of water.
Excessive fluid intake may sometimes lead to diarrhea. However, you’d have to drink a significant amount of water to make this happen — think, upwards of 150 ounces per day for the average person.
Stress
Stress can cause constipation, diarrhea, or other digestive issues. To reduce stress in your life, try:
- Stress-relieving activities such as yoga or meditation
- Regular physical exercise
- Counseling or other types of therapy
- Spending time in nature
- Time with friends and loved ones
Medical Conditions and Medications
Some conditions and medications cause abnormal poops as a side effect.
The most common medical conditions that change bowel function include:
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease (IBD), including Crohn’s Disease and Ulcerative Colitis
- Celiac Disease
- Gastroenteritis (inflammation of the stomach and intestines)
- Diverticulitis (inflammation of the diverticula in the colon)
- Hemorrhoids
- Constipation
- Diarrhea
- Colorectal cancer
- Malabsorption syndromes (e.g., lactose intolerance or fructose malabsorption)
- Gallbladder issues (e.g., gallstones or cholecystitis)
- Pancreatitis (inflammation of the pancreas)
- Liver disease (e.g., hepatitis, cirrhosis, or liver failure)
- Gastrointestinal bleeding (e.g., from ulcers, polyps, or cancer)
- Food intolerances or allergies (e.g., gluten or dairy intolerance)
The most common medications that may alter your poop’s appearance include:
- Antibiotics (can cause diarrhea or changes in stool color)
- Nonsteroidal anti-inflammatory drugs (NSAIDs) (may lead to gastrointestinal bleeding, causing dark or black stools)
- Laxatives (can cause loose or watery stools)
- Antidiarrheal medications (e.g., loperamide, may result in harder or less frequent stools)
- Antacids (containing aluminum or calcium can cause constipation, while magnesium-based antacids may cause diarrhea)
- Opioid pain relievers (can cause constipation and hard stools)
- Proton pump inhibitors (PPIs) and H2 blockers (used for acid reflux or GERD, may cause changes in stool consistency)
- Metformin (used for type 2 diabetes, may cause diarrhea)
- Chemotherapy drugs (can lead to diarrhea or constipation)
- Colchicine (used for gout treatment, can cause diarrhea)
- Orlistat (weight loss medication, may cause oily or loose stools)
- Beta-blockers (used for heart conditions and high blood pressure, may cause constipation)
- Calcium channel blockers (used for high blood pressure and heart conditions, may cause constipation)
- Iron supplements (used to prevent anemia, especially during pregnancy)






![Why Does My Poop Smell Sweet? [Infants & Adults]](https://poopquestions.com/wp-content/uploads/Sweet-Smelling-Poop-Header-768x513.png)
